Transplants
Living livers: how to extend the transplant window
Livers to be transplanted can only survive outside of the body for around 12 hours. But scientists have developed a perfusion system which could extend this to a whole week. Natalie Healey speaks to Professor Pierre-Alain Clavien about what this development could mean for patients on the transplant waiting list in future.
I
f you’re unlucky enough to need a liver transplant, you face stiff competition. This organ is in high demand. The average wait for the master detoxifier is 145 days in the UK, and in the US, around 17,000 people need a new one. Eight patients with conditions, such as end-stage liver disease die every day on the waiting list there.
Aside from shortages, a big challenge with liver transplantation is that the organ has a very short lifespan outside of the body. Standard practices can only keep it alive for 12 hours tops. That doesn’t leave surgeons much time to make the switch. It means any donated liver past its prime has to be disposed of rather than used to save a life.
“Most livers are just kept in the cold at around four degrees. You can use them for up to 12 hours. But, you have to go quickly,” says hepatology specialist professor Pierre-Alain Clavien, chairman of the Department of Surgery and Transplantation at the University Hospital Zurich (USZ).
When you consider the logistics, 12 hours doesn’t sound very long at all. Doctors have to first remove the organ from its donor before prepping the liver for transport to a recipient that could be hours away. And of course, only once the organ has reached its destination can the operation begin.

A scientist places a liver on theLiver 4 Life project’s machine. Image: USZ.
Let livers heal themselves
Last year, a team of scientists developed a machine that could extend the survival window for livers outside of the body to a day and a half. The Harvard Medical School researchers were able to lower the organ’s temperature to a frosty -4 degrees without forming damaging ice crystals. This technique allowed the liver to be preserved for longer than usual. It was important, impressive work but Clavien wanted to push that limit even further. He was determined to develop a perfusion machine that would give a damaged liver enough time to actually repair itself.
“Livers that repair themselves would significantly boost the number of organs available for transplant.”
“Our general idea was to extend it to one week because that's the time you need to regrow part of the liver,” he explains.
Livers that repair themselves would significantly boost the number of organs available for transplant. The initiative — called the Liver 4 Life project — was developed under the Wyss Zurich institute, which brought together experts from Clavien’s team at USZ, along with researchers at ETH Zurich and University of Zurich (UZH). Five years on from that initial idea and after numerous experiments with pig livers, the scientists have reported success.
In January 2020, the team announced in Nature Biotechnology that they’d been able to keep donated human livers alive for seven days with their machine. Ten human livers that had been turned down for transplantation because they were of poor quality were observed on the device. At the end of the week, all of the livers had shrunk and four of them had deteriorated, however, the remaining six were deemed suitable for transplantation.
Clavien explains that about half of all organs that are donated can’t be transplanted because they’re not in good enough condition. “Instead of the organ being discarded, we can put it on the machine and hopefully it will behave well and then we can transplant. So we will save patients on the waiting list,” he says.
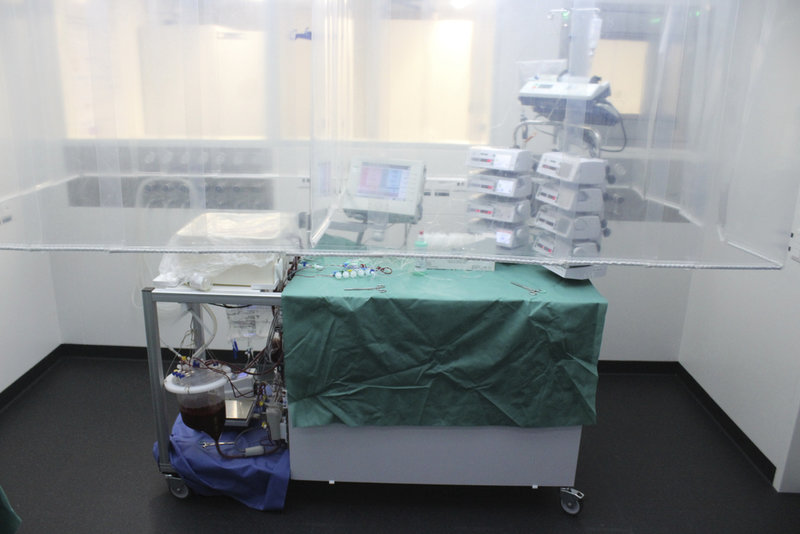
The perfusion machine can keep human livers alive outside of the body for up to a week. Image: USZ.
Mimicking the body
So, how does the liver repair machine work? The basic idea is a perfusion system that mimics the core functions of the human body. “We try to trick the livers that are outside the body into believing that they are still in there,” says Clavien.
But, trying to recreate a similar physiological experience to the human body isn’t easy. And he admits there were several hurdles the team faced at the beginning of the project. Red blood cells placed in the machine would die after a few hours and the lack of oxygen would damage the liver. To get around this, the scientists use a special pump system to provide oxygen and nutrients.
The device also maintains a pressure similar to that found within the body. It even features artificial organs such as a heart, lung, and diaphragm. Everything is automatically adjusted by algorithms, so the technology doesn’t require constant supervision.
“We try to trick the livers that are outside the body into believing that they are still in there.”
The next step for the research is to see if these repaired livers can survive transplantation. One challenge is that some aspects of liver function can’t be assessed until months after they’ve been donated. Clavien says he is currently in conversation with the regulatory bodies about the extra data required before human transplantation with livers perfused on the machine can commence.
In the much longer term, he is intrigued by the idea of auto-transplantation, where a new organ could potentially be grown from a small piece of the damaged one and transplanted back to the original donor. A patient with inoperable liver tumours could have a new organ made from a tiny part of the old one, for instance. It would remove challenges around transplant rejection and the need to take immunosuppressants. “Of course, it’s still science fiction right now, but that’s certainly the long-term goal,” Clavien confirms.