T
he power of needlework should never be underestimated. Where would we be without the textile industry providing natural and synthetic fibres to thousands of sectors across the globe? In addition to clothing our bodies, textiles are used to help heal them, from wound dressings to sutures and meshes. Some scientists are now going further, using weaving and knitting techniques to create medical fabrics from biological materials such as human cells.
Nicolas L'Heureux, director of research at INSERM, the French National Institute of Health and Medical Research is exploring exactly this. He works on repairing damaged blood vessels with biological textiles grown in the laboratory.
“Synthetic materials are recognised as not being a normal part of the body,” L’Heureux explains. “Except for hard metals like stainless steel, gold and titanium, most create a very significant scarring response.”
He likens it to a splinter. The body recognises the material as foreign and reacts to it by trying to push it out. If it’s not able to eject it, scar tissue will form and inflammation will be triggered. This can lead to redness, pain, swelling and scarring.
Some parts of the body are better at dealing with scarring than others. Sometimes a scar can actually be helpful, providing mechanical support to the structure. But in a blood vessel, a scarring response could recreate the same blockage surgeons were aiming to fix in the first place. Grafting and stenting can result in restenosis (where the treated vessel closes off again) over time due to this scarring behaviour.
“A scarring response will create a lot of tissue that will clog the inner part of your tube. Then your blood will not flow well anymore,” L'Heureux says.
Synthetic grafts work best for large vessels such as the aorta, which is roughly two centimetres in diameter. If there is a little bit of scarring from the graft, the blood will likely still be able to flow normally. But for smaller blood vessels, rejection of synthetic materials can create a real problem.
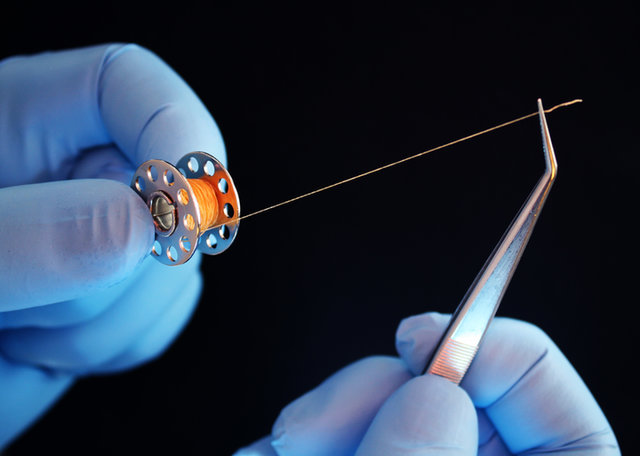
The researchers use collagen sheets to make yarn. Image: Nicolas L’Heureux
Collagen sheets
L’Heureux and his team are developing grafts that won’t produce that rejection response. What is more likely to be accepted is a material the body is already familiar with. Researchers cultivate human cells in the laboratory (originally extracted from a skin biopsy), where various chemicals are used to influence them to form sheets of collagen. These sheets are then cut into thin threads of yarn-like material.
“The material we collect in sheets is the extracellular matrix outside the cell. That's what we get the cells to overproduce in the lab,” L’Heureux reveals. “This is the material that they lay down in the right conditions at the bottom of the plastic containers where we grow the cells.”
Because the makeup of collagen doesn't vary from person to person, it is hoped that each patient wouldn't need vessels produced from their own cells.
“We tend to use weaving because it makes a really nice tight wall.”
Once the yarn is ready, it’s time to get sewing. By weaving, braiding or knitting, the team can form tubes of collagen to replace the synthetic structures that are traditionally used in cardiovascular surgery.
“We tend to use weaving because it makes a really nice tight wall which is really important if you’re making a blood vessel,” says L’Heureux.
This is weaving as you’ve never seen it before, but it still requires a loom. The custom-made device has to be tiny so vessels of five millimetres in diameter can be produced. It’s made out of stainless steel and plastic so it can be cleaned easily. And it is circular in shape to produce tubes from the collagen yarn.

Made entirely from biological material, these blood vessels would be well tolerated by all patients. Image: Nicolas L’Heureux
Testing the textiles
How well these grafts will be tolerated by the body still needs to be tested though. The next step of the research is to see how the vessels perform in animals. Using genetically modified rodent models that don’t reject human tissue, the team will be able to see if the biological textiles adapt well to the body environment.
But one problem with rats and mice is the small size of their blood vessels. So, the researchers are also working on producing similar medical textiles using sheep cells. Once animal model results prove promising, it’ll be time to think about transplanting the grafts into humans.
“We’ll have a solution that we’ve never had before in medicine.”
“The sheep is about the same size as a human in terms of the blood vessels, so we'll be able to try surgeries that we would do in humans with vessels that would be the same size and using all the same instruments. So, it's much more representative,” L’Heureux explains.
There are other research groups working on similar projects. The University of Minnesota Medical School recently grew human-derived blood vessels in a pig. While US company Humacyte is also trying to produce extracellular matrices for vascular and non-vascular applications. In the future, L’Heureux hopes to collaborate with groups like these to find the best way of producing biological textiles at scale.
“When we bring this material that is completely logical, completely human and integrates well inside the body to patients, we’ll have a solution that we’ve never had before in medicine.”