Innovation
Future diabetes care: deep brain stimulation and implanted insulin
Diabetes is a common condition which can be easily managed, but monitoring insulin intake can still be a constant hassle. Now, French start-up Diabeloop has developed a system which combines machine learning with a continuous glucose monitor and an insulin pump to automate the process. How exactly does the tech work, what other innovations are taking place in the field of diabetes care? Chloe Kent reports.

D
iabetics can be divided into two distinct categories – type 1 and type 2. Type 1 is an autoimmune condition, where the body attacks the pancreas and it cannot produce any insulin. Type 2 diabetes patients are either unable to make enough insulin, or produce inefficient insulin. Type 2 is typically brought on by poor diet and other lifestyle factors.
While type 2 can be controlled and brought into remission through eating well and exercising, type 1 will require a lifelong regime of blood sugar testing and insulin administration.
Traditionally, this is done through a finger-prick test where a patient can see if their blood sugar levels are too high or too low. Carrying out these tests multiple times a day can be a substantial mental and physical burden for diabetics, and many medical device manufacturers are now working on alternative options.

Image courtesy of Diabeloop
Artificial pancreas
Diabeloop’s DBLG1 system combines a continuous glucose monitor (CGM) with a patch insulin pump and a dedicated handset which houses an artificial intelligence (AI). The AI connects with the sensor and the insulin pump using secure Bluetooth.
This creates a system known as an artificial pancreas, where a monitor, pump and algorithm work in conjunction with each other to manage a patient’s diabetes automatically without them needing to administer insulin themselves.
The CGM senses and monitors the patient’s blood glucose every five minutes, analysing the data in real time and injecting the necessary dose before the patient is even aware they need insulin. Since the AI monitors daily insulin injection patterns over time, it is able to learn the optimal parameters for each individual patient.
A trial of 68 patients published in the Lancet Digital Health journal found that the DBLG1 system kept patients within their target glucose range 69% of the time. It was also able to decrease the time they spent in hypoglycaemia by 50%.
DBLG1 obtained the European CE mark in November 2018. Diabeloop has entered into a distribution agreement with Dutch firm ViCentra, and the system is now being used in everyday life by around 30 patients.
Implantable insulin
Sernova’s Cell Pouch is an implantable medical device, which can be used to house and protect therapeutic cells inside the body to ensure their long-term survival and optimal functioning. The Cell Pouch can provide a convenient, safe alternative to daily administration of drugs for patients living with long-term conditions – including diabetes.
The Cell Pouch works by transplanting purified insulin-producing islets into the patient, which can produce insulin naturally through a feedback system linking glucose levels to the release of insulin. The device is approximately the size of a business card and can be implanted in a patient through a relatively simple surgical procedure.
The first patient to trial the pancreatic Cell Pouch implant for diabetes showed no adverse events related to the therapy, and was able to maintain blood sugar levels over at least two weeks. They also saw an 88% reduction in the number of hypoglycaemic events they experienced during this period. Simulated blood levels of C-peptide, a biomarker of the pancreas’ effectiveness in responding to rising glucose levels after eating, and insulin were observed 90 days after the transplant in a mixed meal tolerance test.
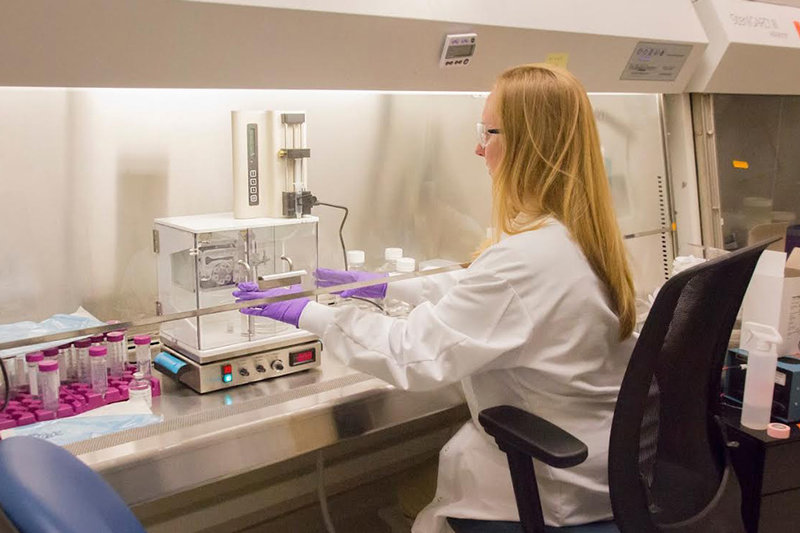
Image courtesy of MIT
Hydrogel beads
MIT offshoot Sigilon Therapeutics is working with Eli Lilly to develop implantable insulin-producing ‘living drug factories’, made of encapsulated, engineered cells, which can be implanted into a patient’s body to produce insulin.
These ‘factories’ consist of hydrogel beads of 1mm in diameter. The beads enter the body through minimally invasive procedures, and act as a delivery device for insulin. The hydrogel case protects the insulin from the patient’s immune system, so that it doesn’t attack the implanted hormone.
The beads are made of chemically modified alginate, a polysaccharide which lines the cell walls of brown algae. When combined with water, alginate can form a gel which safety encapsulates cells without limiting their function.
The modified alginate is permeable and removes any risk of scar tissue formation around the beads, allowing the efficient transfer of insulin. The beads are also designed to block immune elements like T-cells, which will try and destroy the therapeutic insulin cells inside.
Deep brain stimulation
A patient who recently underwent deep brain stimulation (DBS) for obsessive-compulsive disorder (OCD) discovered the unexpected side effect of his type 2 diabetes being significantly improved. The patient was using medication to manage his condition, and experienced a drastic reduction in his daily insulin take.
DBS is a neurosurgical procedure wherein a neruostimulator, referred to by many surgeons as a ‘brain pacemaker’ is implanted under the patient’s skull. The device is programmed to deliver electrical pulses to specific parts of the brain and can be used to treat OCD, depression and other neurological disorders. DBS for OCD is designed to increase the levels of dopamine, which can help control the brain’s reward and pleasure centres and, researchers believe, impact the way the body metabolises sugar.
This unexpected outcome of the patient’s DBS was investigated further, in a study of 14 people with OCD who did not have diabetes. The devices were shut off for 17 hours, during which time blood sugar levels were monitored. Researchers found that DBS therapy increased the patient’s insulin sensitivity, as turning off the simulators correlated with higher insulin levels.
Researchers have yet to confidently establish the link between the central dopamine system and insulin sensitivity in humans, but DBS could provide a way for diabetics to manage their condition in the future.